Kaiser Permanente (San Diego, CA) earned ECRI Institute's 5th Health Devices Achievement Award for its development of registries for tracking orthopedic and cardiac rhythm management (CRM) implants in its member facilities.
The Health Devices Achievement Award recognizes outstanding initiatives undertaken by member healthcare institutions to improve patient safety, reduce costs, or otherwise facilitate better strategic management of health technology. ECRI Institute
announced the winner and four other finalists for the 5th award in October 2010.
Learn about the other submissions that achieved recognition.
The Concept
| |
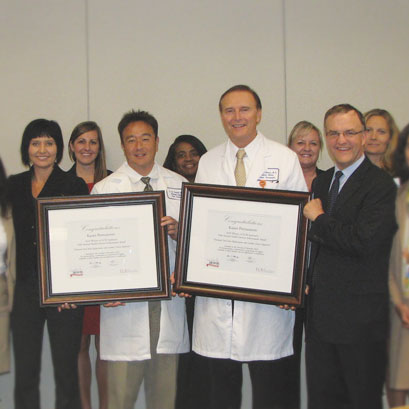 James P. Keller, Jr., ECRI Institute's vice president for health technology evaluation and safety, and director of the Health Devices program (right), presents the award plaques to representatives from Kaiser Permanente, including staff who helped develop the implant registries.
James P. Keller, Jr., ECRI Institute's vice president for health technology evaluation and safety, and director of the Health Devices program (right), presents the award plaques to representatives from Kaiser Permanente, including staff who helped develop the implant registries.
|
Kaiser Permanente started the National Total Joint Replacement Registry (TJRR) in 2001 to track elective primary or revision total knee or hip replacements. The TJRR has grown to become the largest population-based total joint registry in the United States, including over 100,000 cases. Then in 2008, Kaiser Permanente started the Cardiac Device Registry (CDR). Modeled on the TJRR, the CDR includes entries for over 44,000 implantable cardiac defibrillators and pacemakers, covering both initial implants and replacement devices. Between them, the two registries include over 1,000 surgeons and 50 hospitals in Kaiser Permanente's Northern and Southern California, Hawaii, Northwest, Mid-Atlantic, and Colorado regions; Kaiser Permanente plans to expand use of the registries to its remaining regions—Ohio and Georgia.
The motivation behind the implant registries is to (1) reduce costs and improve patient care by reducing the number of revisions for orthopedic implants and (2) help physicians and administrative staff select the most reliable CRM implants. The registries have become exceptional tools for identifying best practices, reducing unnecessary surgeries, managing recalls of implants, and cutting costs.
For the TJRR, data is collected at the point of care—in both the clinic and operating room (OR)—using standardized preoperative, operative, and postoperative forms. These forms are used to gather information about patient demographics, implant characteristics, surgical techniques, and clinical outcomes. This information is supplemented by data pulled from other administrative databases, including data on utilization, mortality, diagnosis, complications, length of stay, and readmission rates. The available information is then analyzed to help surgeons and patients decide which implants to use, to identify patients for whom the risks or potential costs make surgery unwise, to ascertain the relative value of joint replacement compared to alternative treatments, to assess the effectiveness of one brand or design of implant over another, and to evaluate the risk of comorbidities such as diabetes and obesity on health outcomes for joint replacement patients.
For the CDR, data is collected in the OR. In addition, each month the manufacturers of implantable cardiac devices provide Kaiser Permanente with updates from the tracking databases that the vendors are required to maintain for their devices. As with the TJRR, additional data is pulled from other databases to supplement the collected information. The CDR is then used to monitor mechanical complications, infections, and premature battery failure, providing information that guides future selection decisions.
Both registries have demonstrated significant benefits. For example:
- In 2009, over 2,500 patients in the registries were affected by recalls of 15 orthopedic and cardiac devices. Because of the registries, Kaiser Permanente was able to immediately identify and notify the patients with affected devices and then monitor the status of the recall. Efficiencies like this have had a significant economic benefit—for example: Before development of the CDR, Kaiser Permanente spent approximately $4,000,000 on patient identification, communication, and clinical follow-up due to CRM device recalls in 2007 and 2008. With the registry in place, the organization reports that the need for such spending has been eliminated.
- By analyzing data from the TJRR, Kaiser Permanente discovered that smaller femoral size was associated with a 2% higher hip revision rate than larger femoral size, that partial knee replacement had a 10% higher failure rate than total replacement, and that a certain uncemented total knee technique was associated with higher revision rates. Kaiser Permanente reports that by acting on these findings, it was able to prevent hundreds of unnecessary surgeries, benefiting patients and saving millions of dollars.
- The availability of hard data on comparative device performance has allowed Kaiser Permanente to make more informed purchasing decisions. For instance, analysis of TJRR data led to the discovery that some high-tech (and more expensive) implants had no better results than normal implants, which led to selecting different implants. And Kaiser Permanente used registry outcome data to develop a device formulary and standardize implant selection, which it reports led to over $2,000,000 in savings from 2009 through 2010.
- Kaiser Permanente was also able to use registry data to identify patient risk factors for postoperative infection, hospital readmission, deep vein thrombosis, and other complications, which resulted in changes in surgical indications and more effective preoperative care.
- The registries have led to the development of evidence-based best practices that are shared with clinicians through administrator meetings, websites, individualized physician practice profiles, site visits, newsletters, e-mails, and national conference presentations.
In short, the orthopedic and cardiac device implant registries provide Kaiser Permanente with a mechanism for calculating surgical revision and complication rates, identifying affected patients and informing surgeons about recalls, identifying evidence-based best practices, and monitoring implant performance and cost. Kaiser Permanente reports that the registries have led to fewer unnecessary surgeries, saved millions of dollars, and contributed to national quality improvement initiatives. We are proud to recognize Kaiser Permanente's initiative with the 2010 Health Devices Achievement Award.
Best Practices for Other Facilities
Kaiser Permanente is in a unique position to create and maintain databases on this scale, since it is both an insurer and one of the largest hospital systems in the country. But the key idea of gathering and analyzing data to identify best practices is one that any hospital or health system can emulate.