It's important that the type of pulse oximetry sensor is appropriate to its intended location on the patient and to the type of patient being monitored. The choice of an inappropriate sensor can result in erroneous oxygen saturation readings, leading to false alarms or to a failure to alarm when a patient is at risk.
Pulse Oximeter Sensor Selection
Although all pulse oximetry sensors perform the same basic function, they vary in terms of where on a patient they are to be placed. For example, a finger sensor may be used for an adult patient, whereas a forehead sensor may be chosen for a neonatal patient. Therefore, sensor designs take into account factors such as the size of the intended site (e.g., finger, foot). For instance, with disposable sensors, the shape and length of the adhesive bandage depend on where they are designed to be applied.
Sensor Application
Often, it's physically possible to put a sensor on the wrong site. For instance, a neonatal foot sensor can be placed on an infant's toe, and it might seem to fit well when used this way. But doing so may produce inaccurate readings because the distance between a sensor's LED and photodetector is based on the dimensions of the body part for which that sensor is designed. Putting a sensor on the wrong site will affect the amount of light that reaches the photodetector, possibly leading to erroneous readings.
Placement is also a concern with forehead sensors. Products designed for a patient's ear, finger, nose, or toe are transmittance sensors, which use red/infrared (R/IR) light that is transmitted through tissue and then detected. However, products designed for the forehead are reflectance sensors—the R/IR signal is emitted, passes through the tissue, and is then reflected back to the detector side of the sensor. Although it's possible to apply an opened disposable finger sensor by laying it flat across the forehead, any saturation readings obtained from doing so may be incorrect.
A similar problem can occur if the sensor is inappropriate for the patient, such as when an adult finger sensor is placed on a pediatric patient's finger. In addition, because patient weight affects the distance that light must travel between the LED and photodetector, using the right sensor for the patient's weight is important. To avoid placement problems, check a sensor's labeling for its intended site, and follow the supplier's directions. Also, check the labeling to determine the patient weight ranges for which the sensor is approved.
Appropriate Alignment of Disposable Transmittance-Based Sensors
Incorrect sensor alignment is a common problem with using disposable transmittance-based sensors and leads to the generation of false readings. When these sensors are applied, the LEDs and photodetectors should be aligned directly across from one another. (See the figure.)
|
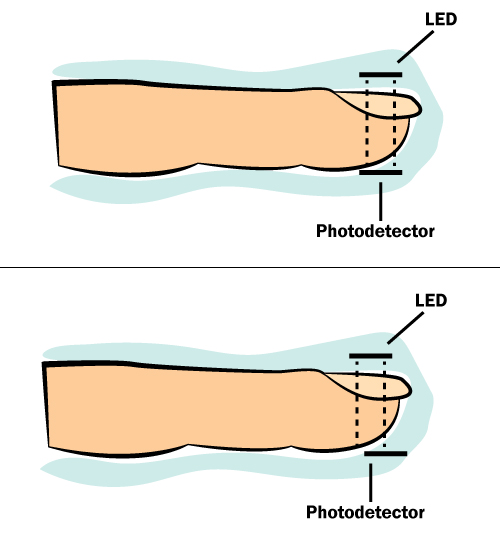
A finger with a disposable adhesive sensor attached. Top: A properly applied sensor. The LED and photodetector are correctly aligned. Bottom: An improperly applied sensor. The LED and photodetector are misaligned, which can lead to problems such as optic bypass. |
Applying the sensors in this way enables the maximum amount of emitted light from the LED to be sensed by the detector. If an LED and photodetector are misaligned, hospitals may encounter a problem known as optic bypass, which occurs when the light emitted from the LED doesn't properly pass through the tissue's arterial bed before reaching the photodetector. There are markers on most adhesive disposable sensors to indicate when the LED is properly aligned with the photodetector. (Clip-on, reusable finger probes are constructed with the LED and photodetector already aligned.) Note that this is not just a concern during application: Once a sensor is on a patient, clinicians should periodically check it to ensure that proper alignment is maintained.